Tiers, deductibles and costly prescription drugs
Published 5:00 am Thursday, March 20, 2008
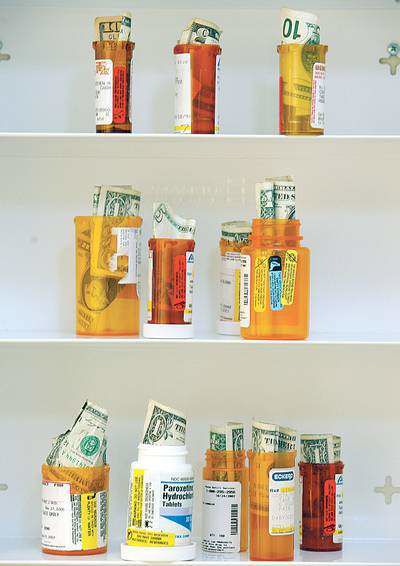
- Prescription drug prices vary in part because of the tier, or level of cost, they are put on by an insurer.
Why do prescription drugs have different co-pay amounts?
If you have insurance, there are a number of different things that affect how much you will pay for a prescription. The plan’s deductible, formulary and tier system all play a role in determining what you will have to fork over at the pharmacy counter.
The deductible is the amount of money you have to pay before the health insurance plan begins to pick up costs. The average deductible last year ranged from $400 to $1,729, depending on plan type, according to the nonprofit research group the Kaiser Family Foundation. Sometimes prescription drug costs apply to a deductible, though some plans place prescription benefits outside the deductible and some have a separate deductible for them.
When the plan begins assisting with the cost of drugs, you will often be required to make a co-pay, the part of the drug’s cost that you must pay. That co-pay may vary based on whether the drug is in the plan’s formulary.
Drug formulary
A formulary is a list of drugs for which the insurer has decided to offer discounts, sometimes also called a list of covered drugs. Formularies, said Dr. Joseph Johnson, medical director for Clear Choice Health Plans in Bend, allow insurers to keep costs down by not offering every drug. “The formulary is just a way of narrowing the universe.”
It is possible, though not always easy, to get a list of your plan’s formulary by calling the insurer. Make sure to have your group or policy number; different policies often have different formularies.
Plans can have open formularies or closed formularies. An open formulary means that, even if the drug isn’t listed on the plan’s formulary, you will likely get a discount by using your insurance card.
A closed formulary means that, if you get a drug that is off the formulary, you likely will pay the same price as a person who does not have insurance. For some drugs, especially generics now offered for less than $5 by large chains, it may not make much difference whether or not the drug is on the plan’s formulary. For more expensive or brand-name drugs, sticking with the formulary could save considerable money.
Price tiers
Formularies are often divided into tiers, with drugs at higher tiers costing more than drugs at lower tiers. Tiers are a way for insurers to get beneficiaries to pick up some of the costs of expensive drugs and steer them into lower-cost prescriptions when possible.
“One of the ways to get individuals to pick up more cost-effective medications is to put the drugs in different tiers,” said Johnson.
More than three-fourths of Americans who get insurance from their employers, or about 2.5 times the number who did in 2000, have drugs divided into tier systems, according to the Kaiser Family Foundation.
Generic drugs are often on the lowest cost tiers, with co-payments usually about $10. The second tier usually includes preferred brand-name drugs, said Johnson. Those, said Johnson, include drugs that the insurer has negotiated with the drug company for a discount or drugs that are known to work particularly well for a certain condition.
Most plans include a third tier, and many, including the most popular Medicare Part D plans, include a fourth tier as well. The higher tiers, said Johnson, include the most expensive drugs or the ones for which there are cheaper alternatives. For example, Johnson said, many of the Clear Choice plans put Nexium, used to relieve acid reflux, in the third tier because there is little data to show that it is more effective than the cheaper over-the-counter alternative, Prilosec.
In the higher tiers, particularly for those on Medicare Part D plans, people are often required to pay a percentage of the total cost of the drug. For some drugs, that can run in the hundreds of dollars per month, and the tier system has been criticized for making certain treatments prohibitively expensive. Most private employer-sponsored plans still use co-pays, with the average co-pay for the highest tier at $43, according to a 2007 survey by the Kaiser Family Foundation.
Johnson said the system is necessary to keep down the cost of health plans.
“We could give people all those things,” he said. “But then the premiums would be high. … Then you get into a situation where it’s just too expensive.”
Still confused? Talking to a pharmacist or your doctor about ways to reduce your prescription costs can sometimes help. Often, a doctor can prescribe a lower-cost drug or a pharmacist can suggest something that will cost less. There are also some government or private programs that can reduce the costs of your prescriptions.






