For patient pain, drug treatment divides doctors
Published 5:00 am Friday, August 8, 2008

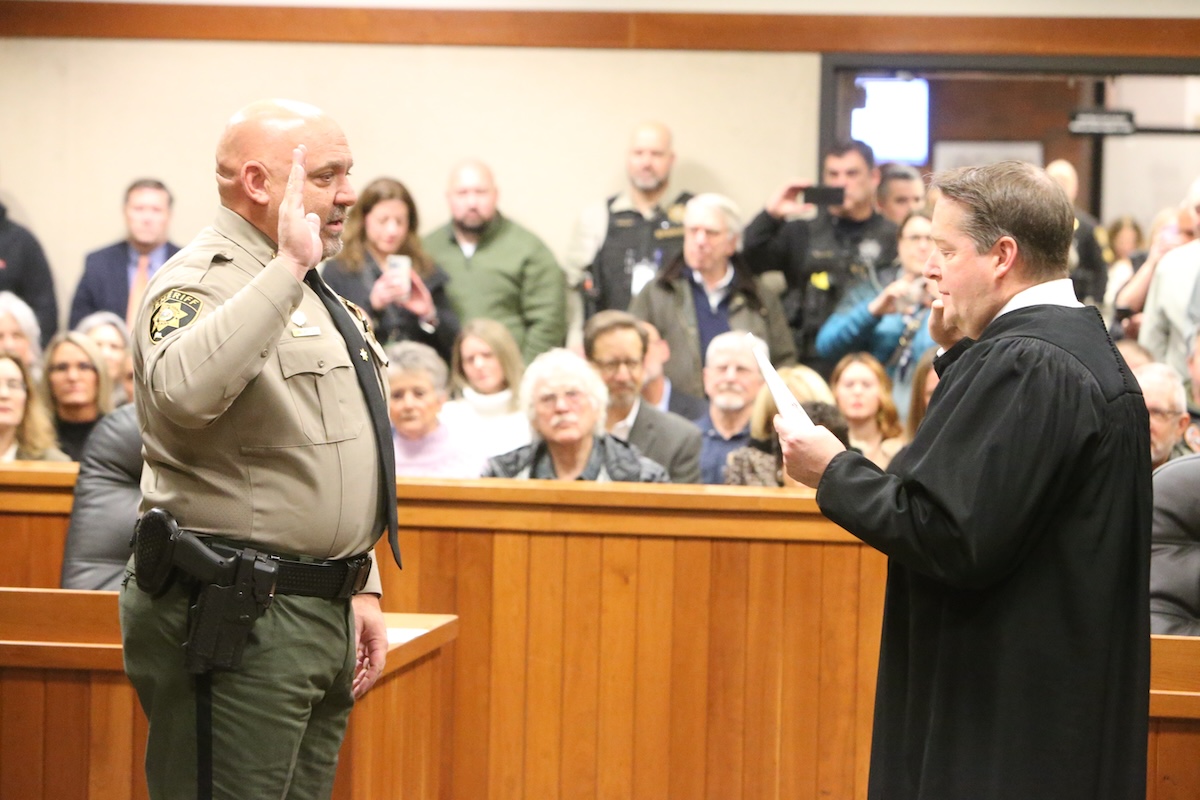
- Dr. William Witt, a pain-management specialist, treats Patsy Florence in his office in Lexington, Ky. Witt does not prescribe narcotics for chronic pain because he says no studies show improved function and pain relief beyond six months.
LEXINGTON, Ky. — Many doctors are wrestling with questions of how and when to treat thousands of legitimate patients who need narcotics.
It’s all part of perhaps the hottest national debate in medicine today.
The discussion revolves around two camps. One holds that pain essentially is an illness in its own right that should be treated aggressively, up to and including the use of powerful narcotic drugs. The other side contends that doctors must be much more conservative, offering narcotics only when they’re absolutely sure patients actually need the potentially addicting drugs and are not seeking them to abuse them.
Some nationally known experts, like Dr. Russell Portenoy, a New York pain specialist, say the debate has left many doctors reluctant to prescribe narcotics because they fear being investigated by authorities and many patients reluctant to seek help because they fear being seen as “pill users.”
“The drugs are highly stigmatized,” Portenoy said in an interview. “Doctors who prescribe them are stigmatized by their colleagues; patients who use them are stigmatized by their families, their friends and by other doctors.”
The debate is followed closely by many physicians in Kentucky, where prescription drug abuse is a perennial problem and where several doctors have gone to jail in recent years for running highly profitable “pill mills” that cranked out prescriptions to those who abused or sold them.
Just about everybody involved agrees that pain is a serious national health problem.
It is estimated that between 40 million and 80 million Americans suffer from chronic pain — defined as pain that lingers for six months or more — and that many are at least partially disabled as a result. By some estimates, the problem costs America $100 billion a year in medical costs and lost productivity.
Nevertheless, experts such as Dr. Barry Cole, executive director of the American Society of Pain Educators, say millions of sufferers don’t get proper relief.
The reasons, Cole says, include lack of health insurance, which hinders patients in getting treatment, and doctors who are either afraid to prescribe the necessary drugs or who lack the training to dispense them properly.
“Basically, about every sixth American suffers from pain every day,” Cole said in an interview. “If this were cancer, if this were heart disease, if this were HIV, it would be considered the number one health concern in the country. That’s the insanity of all this.”
Chronic vs. acute
Dr. William Witt, chairman emeritus of anesthesiology at the University of Kentucky and a pain-management specialist, says physicians agree that it is proper to prescribe powerful narcotic drugs to treat patients with acute post-surgical pain or pain from illnesses such as cancer.
The debate, Witt said, is about using those drugs to treat patients suffering from chronic, ongoing pain that can stem from many sources, some that are not easily diagnosed.
Witt says he doesn’t fault doctors who prescribe narcotics for chronic pain, but he doesn’t prescribe them himself because scientific evidence is lacking.
“There are virtually no studies that show improved function and pain relief from these drugs beyond six months,” he said. “We’re also starting to recognize that when you give these drugs at high dosages over a long period, they actually start to produce pain.”
Witt also contends that the risk of addiction can be high — “There’s a reason these drugs are controlled,” he said — and that other, non-narcotic approaches are available to help patients with severe long-term pain.
“Here at the university we don’t use opioids (narcotics) for chronic pain at all, and we treat lots of pain patients very effectively,” Witt said.
Alternative methods include non-narcotic drugs, physical exercise and electrical impulse devices to ease pain, he said.
On the other side of the argument are doctors such as Portenoy, chairman of pain medicine and palliative care at Beth Israel Medical Center in New York, who think narcotics can be safely and effectively prescribed for chronic pain. Portenoy agrees, however, that supporting scientific evidence still is lacking in many areas.
“Having said that … it’s now the consensus in the pain specialty community that opioids are appropriate for a carefully selected subpopulation of chronic pain patients who can benefit with tolerable side effects and with no problems of abuse,” Portenoy said.
Identifying those patients, however, isn’t easy.
For one thing, most patients with chronic pain end up seeking help from primary care physicians because there are only about 10,000 to 12,000 pain specialists to serve the entire country.
Barbara Hunter, a Lexington attorney who represents people with disabilities, also points out that patients who lack health insurance often can’t get in to see pain management specialists.
But primary care doctors might lack the time — and the training — to adequately evaluate patients seeking help with chronic pain.
Add in the possibility that some of those patients might be faking to get drugs for abuse or resale, and the risk of doctors being duped is high.
In one case reported in Florida earlier this year, a pain doctor who is meticulous about screening patients was fooled by an 80-year-old woman who sold the drugs to supplement her husband’s monthly Social Security check.
Even experienced doctors can be taken in, says Dr. Roger Humphries, chairman of emergency medicine at the University of Kentucky. He says that leaves doctors in a ticklish situation.
“It can be very confusing to sort through who is there for an acute pain condition, who’s there for a chronic pain condition, and who is there for something that is more of a drug addiction problem,” Humphries said. “Very often, we have to give the patient the benefit of the doubt. It’s an issue emergency physicians struggle with daily.”
Humphries said he would “rather be duped by someone seeking narcotics … than to neglect to give medications to someone who really needs them.”