Excercise-induced asthma
Published 5:00 am Thursday, April 21, 2011
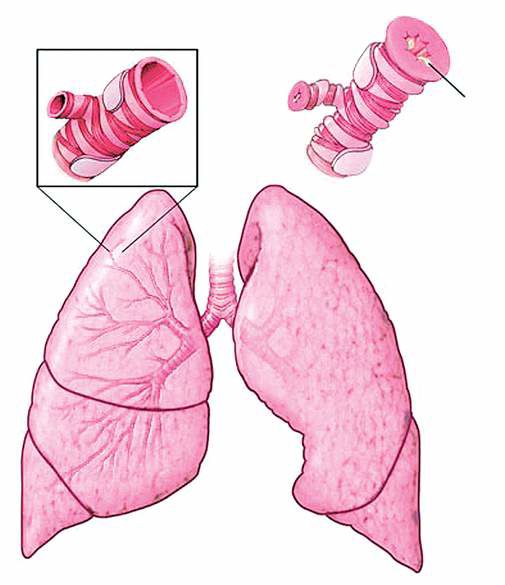
- Asthma Attack: During an attack, inside walls of the airways in the lungs can become inflamed and swollen. Membranes in the airway linings may secrete excess mucus. The narrowed airways make it harder to breathe and trigger coughing and wheezing. Source: Mayo Clinic
When Dakota Blackhorse-von Jess ran competitively at Mountain View High School, he was used to having a tight chest during a race.
After all, it’s pretty normal for competitive endurance athletes to push themselves to the edge, to the point they can hardly breathe, he said. So he thought nothing of it.
“It was my racing paradigm. I didn’t know asthma was my problem,” he said. That is, until one day when a runner friend with similar symptoms offered Blackhorse-von Jess his inhaler.
“It’s not something I would have realized until someone pointed it out,” he said.
With exercise-induced asthma, or bronchoconstriction, hard breathing from any kind of intense exercise — swimming, running, basketball — triggers the breathing airways to tighten and produce extra mucus, leaving less room for air.
It’s a common problem that can affect people of any age and during a variety of endurance activities, although it’s more prevalent in serious athletes. It can happen in people who don’t otherwise have asthma or allergies, and there’s a scale of symptoms from annoying to dangerous.
Now 25, Blackhorse-von Jess is a strong and competitive cross-country ski racer. Most of the time, two puffs on an albuterol inhaler before a hard workout or race will minimize symptoms. Asthma is not restricting his life or his training, he said.
Unless you count that time he passed out during a race.
Exercise-induced asthma is notoriously worse in cold air. During a national ski race this winter, Blackhorse-von Jess’ lungs began to clench up tighter and tighter.
He thought he could push through it as he had done so many times before. Eventually about halfway up a climb, his lungs “locked up,” he recalled. He crested the hill, then blacked out and lay down in the snow. Clearly, he lived to tell the story.
Dr. Adam Williams, an allergy, asthma and immunology specialist at Bend Memorial Clinic, said in only very rare cases is exercise-induced asthma fatal. Typically those cases are when asthmatics exercise hard at times they shouldn’t, such as when the air is thick with wildfire smoke, or when they have an underlying viral illness.
Generally speaking, Williams said, 8 percent of the country’s population has regular asthma, a medical condition that is often genetic. Coughing, wheezing, chest tightness and pain, difficulty breathing and fatigue can be triggered in a person with regular asthma by pollens, dust, viruses, cold air, pollution, exhaust or cleaning supply fumes, to name a few.
For about 90 percent of those people with regular asthma, exercise can be one of the many potential triggers of those symptoms.
Separately, Williams estimated that 5 to 10 percent of the population has exercise-induced asthma. They experience those unpleasant symptoms exclusively when they’re breathing hard during endurance exercise. Exercise-induced asthma seems to be growing, said Williams.
Why? Overall, he said, asthma and allergic conditions in general are rising. There are various theories to explain their growth, including the hygiene hypothesis, which says that a lack of early childhood exposure to various microorganisms and parasites suppresses the development of the immune system and makes people more susceptible to health problems.
And, as for exercise-induced asthma specifically, growth could be attributed to the fact that “more people are exercising,” Williams said. He has read studies from the 1970s that refer to “this new fad of exercise taking off,” he said.
Some research says the large volume of air breathed by elite athletes can cause some adults to develop exercise-induced asthma, Williams said. Perhaps they’re breathing in more irritants over time, even if they’re not genetically predisposed to asthma, he said.
Some studies have indicated that consuming more ascorbic acid (vitamin C) and eating more omega-3 fatty acids and less sodium can help reduce the symptoms. Williams hasn’t prescribed these things to his patients. He said the albuterol inhaler is easy and effective. It requires a prescription. The inhaler relaxes muscles that surround bronchial tubes and dilates the airways for four to six hours. Inhalers come with possible side effects such as a racing heart rate or a jittery feeling. And the inhaler shouldn’t be overused or a tolerance will build up, rendering it ineffective, he said. Williams also said some athletes can reduce their symptoms by taking more time to warm up or by starting off more slowly.
But in no case should exercise-induced asthma keep someone from exercising, he said. If slow warm-ups or inhalers don’t work, there are additional things to try, including inhaled steroid medications and other drugs.
“Everyone should be able to achieve a high level of exercise and not be slowed down by exercise-induced asthma,” he said. “Exercise is so important for health, and the medicines we have are so effective. There’s no excuse.”
Michael Dennis, of Bend, has lived with exercise-induced asthma since high school, and he gets out for some exercise most days of the week. He said he used to cough a lot with particularly intense efforts, but over time his symptoms worsened to include chest tightness and shortness of breath, enough to affect his performance while Nordic skiing, running or biking. Now 35, Dennis does a lot of road biking and cyclocross. Like most people, his symptoms are worse in the cold.
He’s used an albuterol inhaler before, during or after exercise, which “for the most part” alleviates the symptoms. A good, slow warm-up session before a hard effort is also effective, he said.
“Fortunately, I haven’t had to adjust my workout routine much,” he said. “I have had only a few true asthma attacks where I felt I was having difficulty getting enough air, one during the swim portion of a triathlon, and as long as I do the appropriate prevention, I have been able to maintain the lifestyle that I desire.”
Asthma Attack:
During an attack, inside walls of the airways in the lungs can become inflamed and swollen.
Membranes in the airway linings may secrete excess mucus. The narrowed airways make it harder to breathe and
trigger coughing and wheezing.
Source: Mayo Clinic






