Making the leap to a private exchange
Published 12:00 am Thursday, November 28, 2013
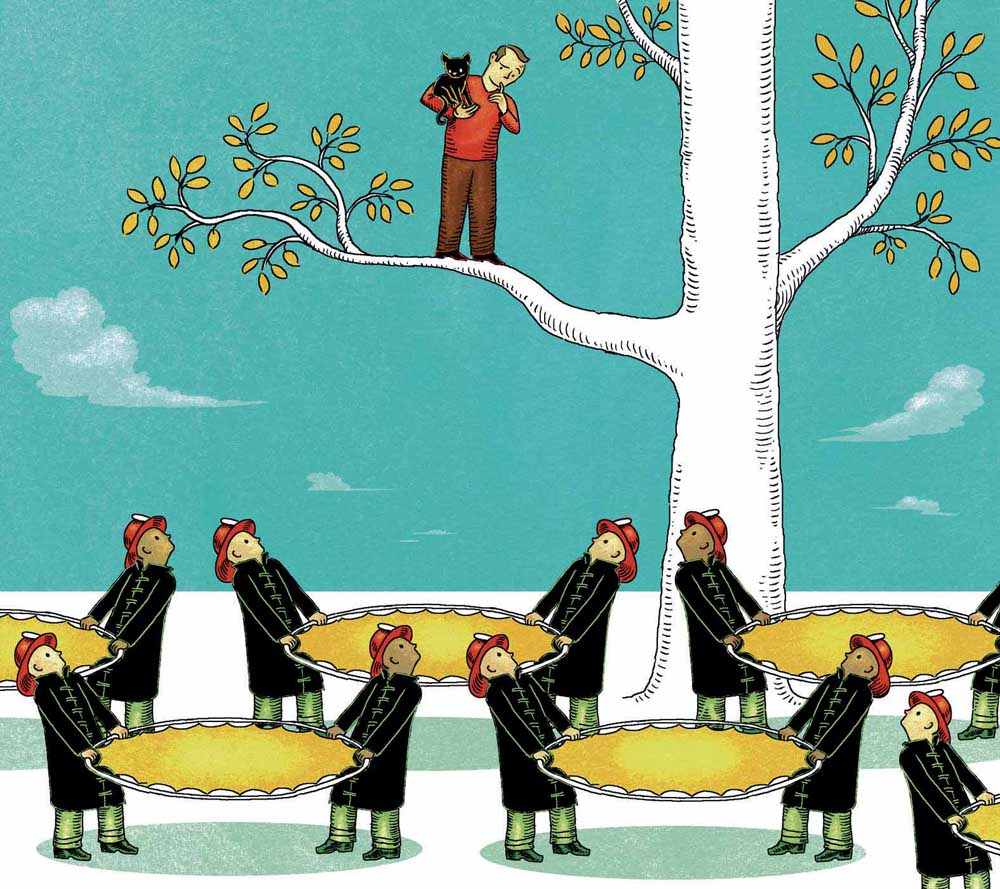
- Illustration by Wesley Bedrosian / New York Times News Service
The troubled rollout of the federal health insurance marketplace this fall has given the word “health exchange” a bad name. Nonetheless, some companies are choosing to offer their employees health benefits via private exchanges — online insurance marketplaces that are separate from the federal system.
This month, for instance, about 180,000 workers eligible for health benefits at Walgreens are choosing their plans on a private exchange for the first time. And workers at Sears Holdings just completed their second enrollment period using an exchange.
Private exchanges are just one of the changes employees are seeing this year during open enrollment season, when employees with workplace health coverage choose their plans for the coming year. Other trends this year include plans with higher deductibles, sometimes accompanied by a tax-advantaged health-savings account; a shift away from employer coverage of spouses who could get insurance through their own jobs; and programs that offer financial incentives for employees to take steps to improve their health.
The changes are happening as employers seek to control costs amid a roiling health care system. New rules under the Affordable Care Act require companies with 50 or more workers to offer affordable health coverage or pay a penalty. This “coverage mandate” was delayed a year, however, so workers — especially those at small companies, close to the law’s threshold — may see more changes next year.
Some employers may try to stay below the 50-worker threshold to avoid the requirement, while others may simply pay the penalty and send workers to the government exchanges to find health insurance.
A relatively small but growing number of midsize and larger companies that already offer insurance to employees are now shifting to private exchanges — perhaps the most significant change employees have seen in a while. Companies like IBM and General Electric have adopted them for their retirees, rather than active employees. But if the exchanges work well for their initial participants, more companies may shift current workers to exchanges, too.
Accenture, a consulting firm, estimates that 1 million people will enroll in private exchanges this year, but that number could grow to 40 million by 2018.
So far, the exchanges seem to appeal to companies that have a range of employees at varying pay levels — like retail and restaurant companies, which have hourly workers as well as salaried employees — because employers can offer more options in plan design, said Paul Ginsburg, president of the nonprofit Center for Studying Health System Change, which conducts health care research.
Walgreens and Sears participate in the exchange run by Aon Hewitt, a benefits consultant that started the Corporate Health Exchange in 2012 for its own employees and added outside companies for this year. For next year, the exchange has 18 companies with 330,000 employees participating. Including spouses and children, the total covered is about 600,000 people, said Ken Sperling, the company’s national exchange strategy leader. Major insurers like Aetna and UnitedHealthcare are participating.
Other firms offering private exchanges include Towers Watson, Mercer and Buck Consultants. And some insurance companies are expected to start offering their own exchanges.
Details vary, but typically participating employers determine an amount to contribute per employee toward health coverage. That varies by employer. Then, the worker goes onto the exchange to find a plan.
Some experts worry that the new model could make it easier for companies to limit their contributions to their workers’ coverage. But Sperling said that wasn’t happening. Every company participating is paying the same or more than it did in the previous year. “Nobody is using it as an excuse to cut their contributions.”
Michael Polzin, a Walgreens spokesman, said using the exchange would help the company predict costs and offer more choices to its employees. For this year, workers had a choice of four plans — two from two insurers. But on the exchange, he said, workers will have a choice of five insurers, offering up to five plans each. “It comes down to being able to give them more options to better meet their needs,” he said.
Dean Carter, chief human resources officer at Sears Holdings, said the company offered the same level of premium subsidy regardless of the plan employees choose, so those selecting one with richer benefits might have to pay more out of pocket, he said. The exchange uses the same “metallic” rankings as the public government exchange to help employees compare plans from different insurers — platinum plans generally have higher premiums, but lower deductibles; bronze plans have lower premiums and higher deductibles.
Employees see on their paycheck stub what the premium is and what portion Sears is paying. “You know the total cost,” he said.
The result, he said, is that employees seem to be paying close attention to the details of their health plans, including not only its premiums but other out-of-pocket costs, as well as doctor networks.
He said he noticed the change at the company’s annual benefit fair held during open enrollment. In years past, when Sears used a single carrier, employees would come to get key chains and other promotional trinkets from the insurance company. But this year, workers asked insurance company representatives very detailed questions.
“Is my doctor on your plan? How can I get my doctor on your plan? Why is your plan more expensive?” Carter said. Insurance carriers are used to hearing such questions from benefits executives, he said, but not necessarily directly from workers.
Ginsburg said it was unclear whether the new private exchanges would result in the savings companies were hoping for, given the current changes in health insurance industry. For instance, some companies are considering whether they may save money by switching to a “self-insured” model — meaning that the company pays employee health claims itself, rather than being “fully insured” and paying premiums to an insurance company, which pays the claims — in part because self-insured plans are exempt from an insurer tax required by the Affordable Care Act. Yet, some employers moving into private exchanges are switching to the fully insured plans.
Polzin said taking all factors into consideration, Walgreens decided that joining the exchange and switching to a fully insured health plan was the best option. The model, he said, “will give us more certainty of health care costs from year to year and will align the insurers with us to control costs.”






