The Center launches outpatient hip and knee replacements
Published 12:00 am Saturday, April 30, 2016
- The Center launches outpatient hip and knee replacements
About four hours after having his right hip replaced, Bruce Axten took a short walk — a nurse by his side — up and down the hallway outside his recovery room early Monday afternoon.
“I’m way amazed at how I feel right now,” the 51-year-old Bend resident remarked to a reporter about 15 minutes later.
Trending
He was sitting in a recliner, pillows beneath his calves, wearing a T-shirt, gym shorts and tennis shoes. “And it’s not just the drugs. But they help.”
Axten was the fourth patient to receive a hip replacement at the Cascade Surgicenter, the outpatient surgery facility inside The Center Orthopedic & Neurosurgical Care & Research in Bend.
The facility in October became the first in Central Oregon to perform outpatient hip and knee replacements, involved surgeries that typically require at least two nights in a hospital both nationally and statewide.
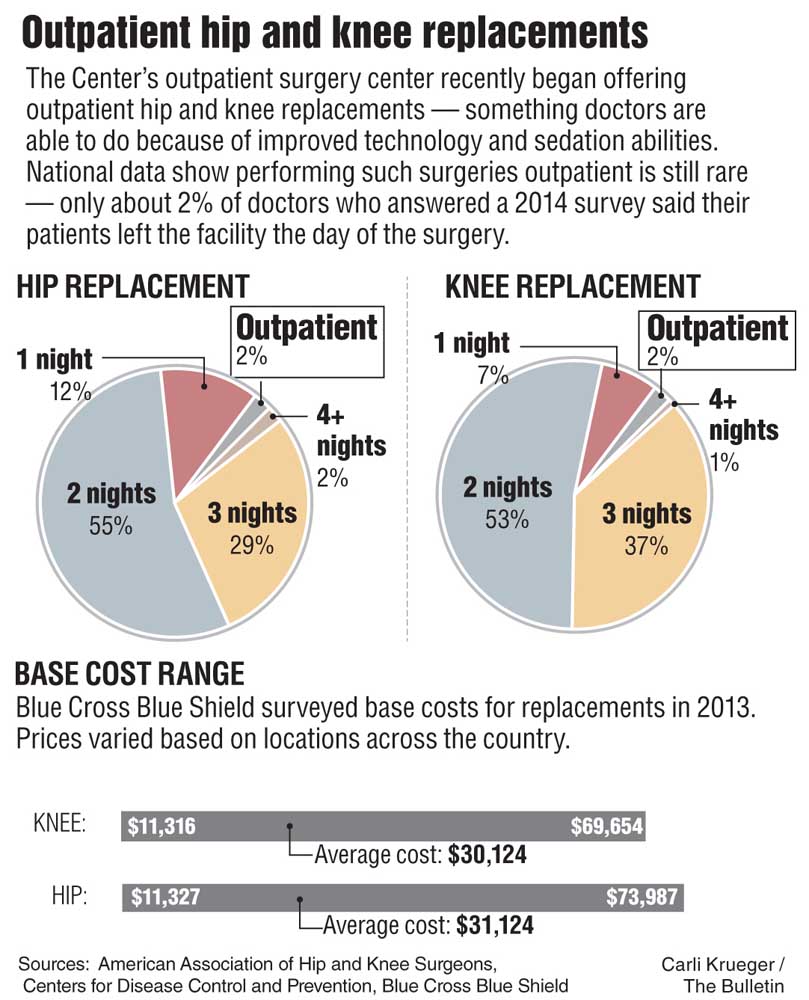
Only 2 percent of surgeons surveyed in 2014 reported performing outpatient hip and knee replacements, according to the American Academy of Hip and Knee Surgeons. The greatest proportion of surgeons — more than half — said their patients stayed in the hospital for two nights.
Dr. Timothy Bollom, an orthopedic surgeon with The Center, called the change a “paradigm shift,” and said it follows the trend of medical procedures becoming less invasive and recovery times becoming shorter.
“Ten years ago, if you got a knee replacement — at least when I was training — we kept patients five to six days,” he said.
Trending
About 719,000 Americans had knee replacements and 332,000 had hip replacements in 2010, according to the Centers for Disease Control and Prevention’s most recent data. They’re most commonly performed on older adults with severe arthritis, a condition that causes pain, stiffness and swelling even during simple tasks like walking or climbing stairs.
A hockey player since he was a kid, Axten said tight hips always kept him from twisting his torso while working the puck.
“My whole life, I’ve never had a good shot and I didn’t know why,” he said.
In recent years, the problem began to affect mundane tasks like bending down to pick up a box. Finally, in December, his doctor delivered the bad news.
“He said, ‘Both of your hips are shot,’” Axten said.
Advances in sedation
Several experts interviewed cited advances in sedation as the key reason patients can leave so quickly after the surgeries. Doctors use a combination of localized anesthesia injections and other forms of sedation that allow patients to more quickly wake up and become coherent after surgery.
The new sedation techniques also decrease nausea.
The surgery itself is the same whether it’s done inpatient or outpatient. But outpatient surgeries require careful preparation beforehand, including a “pre-hab” appointment in which patients learn to use a walker and perform exercises to strengthen their quads, said Cammy Gilstrap, director of the Cascade Surgicenter.
The Bend Surgery Center, which performed its first outpatient knee replacement a few weeks ago, sends physical therapists to patients’ homes before the surgeries to ensure they’ll have a safe, comfortable environment to recover in, said Neal Maerki, the facility’s administrator. The surgery center will do its first hip replacement next month.
Changing patients’ expectations about the surgery is an important step toward allowing them to go home the same day, said Dr. James Ballard, an orthopedic surgeon with offices in the Portland metro area. Telling people they’ll be able to go home the same day gives them the confidence to do so, he said.
“If you approach them and say, ‘Oh my gosh, you are having this big, gigantic surgery. There is no way you can go home for three or four days,’ people are going to stay for three or four days because that’s what they think they’re supposed to do,” said Ballard, who two years ago became the first surgeon in the Pacific Northwest to perform an outpatient hip replacement.
Not all eligible
A minority of patients who need hip and knee replacements will be eligible to have them done outpatient.
Appropriate candidates must be generally healthy and can’t have heart or lung disorders. They also can’t be above a certain body mass index, Bollom said. Potential candidates will also be screened to make sure they have someone to take care of them once they go home.
And the other crucial piece: motivation.
“A lot of patients are motivated not to have to stay in the hospital,” Bollom said, “so those are the patients that kind of come looking.”
On the other hand, not all patients feel comfortable going home the same day, and that’s OK, too, said Dr. Jay Lieberman, immediate past president of the American Academy of Hip and Knee Surgeons.
“I don’t see patients clamoring to go home the same day,” said Lieberman, who also serves as chairman of the University of Southern California Keck School of Medicine’s orthopedic surgery department.
As more facilities perform outpatient hip and knee replacements, Lieberman said he’s concerned patients won’t be properly screened. Picking the wrong patients could result in readmissions to the hospital, which would lead to higher costs, he said.
The trend toward outpatient surgeries is largely driven by a desire to lower costs. Last year, St. Charles Health System charged roughly $44,000 for an inpatient hip replacement and $45,000 for an inpatient knee replacement. The actual costs vary depending on one’s insurance. The Cascade Surgicenter’s base charge for patients who don’t have insurance is $25,000, although Gilstrap said so far, all patients have had insurance. As with any medical procedure, what patients ultimately pay is based on a contract between their insurer and the surgery center.
Maerki declined to provide the Bend Surgery Center’s prices.
Ballard said he’s not sure whether insurance companies have figured out how to pass those savings on to patients, however. He thinks in the future, insurers will create an incentive for having the surgeries done in an outpatient facility by making patients pay a smaller share of the bill.
On top of the lower costs associated with a shorter stay, outpatient surgery centers tend to be more nimble than hospitals. They have lower overhead costs because they don’t have to maintain things like kitchens and pharmacies, Gilstrap said.
In Ballard’s experience, private health insurers were reluctant to cover the surgery as outpatient at first, but almost all have since agreed to cover the procedure once they realized patients were having good outcomes and it costs roughly 30 percent less than if done in a hospital.
Given that demand for hip and knee replacements is expected to skyrocket in the coming decades, being able to perform them for less should be a priority, Ballard said.
“We have too many surgeries that need to be done and too little money to pay for it,” he said.
One of the barriers to outpatient has been the fact that surgery centers weren’t built with hip and knee replacements in mind, Ballard said. The procedures require large operating rooms to hold trays full of equipment, large rooms for cleaning equipment and recovery rooms patients can spend a longer amount of time in, he said. He’s currently in the process — along with a group of Portland area surgeons — of building an outpatient facility that will specialize in hip and knee replacements. Its footprint will double that of standard surgery centers, with bigger recovery rooms, hallways and areas for physical therapy, he said.
Most patients who go to Oregon Health & Science University for knee or hip replacements stay an average of two nights in the hospital, said Dr. Thomas Huff, an assistant professor of orthopedics and rehabilitation. OHSU’s current outpatient surgery center was not designed to perform those surgeries, but Huff said the provider is building a new facility that will specialize in outpatient hip and knee replacements. The project is separate from Ballard’s.
Slow to catch on Although a few physicians have been performing the outpatient surgeries since the early 2000s, the practice has yet to become mainstream. Some say that’s because buy-in from insurers has been slow. Medicare still doesn’t cover it.
Doctors at The Center first discussed the change in 2011, but it took a long time to get health insurers on board. It was the same for the Bend Surgery Center, Maerki said.
Many physicians hope Medicare will agree to cover the outpatient surgeries within the next couple years. Ballard said he thinks that would bump the proportion of eligible patients up to half.
Other doctors were more cautious in estimating how many Medicare patients, most of whom are 65 and older unless they have disabilities, would be healthy enough for outpatient.
Before patients are permitted to leave following the surgery, they have to perform a series of tasks with a physical therapist, such as walking a certain number of feet and climbing stairs, Gilstrap said.
Barbara Harris, who had her right knee replaced at the Cascade Surgicenter in October 2015, was among the first to do so. She recalls being instructed to walk to the bathroom and back. A nurse showed her how to manage stairs, but the 64-year-old Sisters resident wasn’t able to climb them for a few days after the surgery.
A medical technologist for 25 years, Harris said she learned all about the infections people pick up in hospitals. That’s one of the main reasons she wanted to have the outpatient surgery. She said she also knew she would be more comfortable and better cared for at home under the watchful eye of her husband. Both of them are retired.
Harris had cooked ahead of time, and friends brought meals over, but having someone help her around the house was crucial,
“You seriously do need somebody to help you at least 10 days,” she said.
Back at the surgery center, Axten — his wife at his side — had only good things to say about his experience there: easygoing staff, well-controlled pain. He estimated it would be four weeks before he’d be able to drive to his job at Hewlett-Packard in Vancouver, Washington. Luckily, he frequently works from home.
In the meantime, Axten said he was itching to get home in time to watch the hockey playoffs at 5:30. He looked up at his nurse hopefully, who said he’d be able to leave at 4:30. “This is the best staff,” he said.
— Reporter: 541-383-0304,
tbannow@bendbulletin.com
Editor’s note: This article has been clarified to reflect the fact that Oregon Health & Science University’s new outpatient surgery center project is separate from the facility Dr. James Ballard is constructing.