Medicaid population expected to decline
Published 12:00 am Thursday, November 17, 2016
- Medicaid population expected to decline
Within the past two years, Oregon’s Medicaid program took on thousands of new members, pushing its total enrollment to more than 1 million. In the next two, the program is projected to shed more than 60,000 members.
Members who joined the program, called the Oregon Health Plan, under the Affordable Care Act’s expansion to 138 percent of the federal poverty level — $16,394 annual income for an individual — currently number about 409,000. That’s expected to drop by 10.4 percent between 2017 and 2019 to about 355,000.
Trending
The reasons are multifaceted, but a big driver is simply that people aren’t aware they need to reverify their eligibility for the program every year. The Oregon Health Authority, which oversees the program, sends letters to people letting them know, but in many cases, their addresses have changed.
PacificSource Community Solutions, the organization that administers OHP locally, has sent mailers to its members in the past, but more than half of them came back as undeliverable, said Dacia Farley, PacificSource’s manager of Medicaid operations.
“These members tend to move around; phone numbers change,” she said. “So I think maintaining an accurate database of how to contact these members is one of the biggest barriers from all sides.”
Members tough to track down
PacificSource’s membership in Deschutes, Crook and Jefferson counties declined from about 52,000 in September 2015 to about 48,000 in September 2016.
Unlike commercial insurance policies, which people can buy only during a specific time period unless they have a qualifying event, OHP members can enroll any time. Their renewal deadline is one year from the day they joined.
Trending
An address or phone number is not required when applying for OHP, so some people choose not to provide them.
In addition to mailing letters to its members, the OHA also sends regular lists to PacificSource of its members due for renewal.
Instead of contacting those members directly as it used to do, PacificSource now gives the information to their primary care providers, who can either attempt to contact the patients or do nothing.
There’s wide variation in how providers use that list, said Lindsey Hopper, PacificSource’s vice president of Medicaid.
“You’ll find some providers who do not see that as being a good return on time investment and others who are putting more time into it,” she said.
Weeks Family Medicine, a medical clinic in Bend, has a full-time staff member who’s sole job is to track down OHP patients and make sure they renew, said Jaimi Weeks, the clinic’s CEO. She estimates the clinic is losing about 10 percent of its OHP patients every month.
“We do not want to turn away any patients,” Weeks said, “but if they haven’t even turned in their applications, then we don’t know what to do.”
Weeks said she wishes the coordinated care organization, or CCO, would do more to help providers contact their patients. Oftentimes, providers have more current information about the patients than the OHA, especially if they’ve been to the doctor recently. Weeks suggested providers could add contact information to the patient lists they receive and return the updated list to PacificSource.
“Calling these people is tedious and unsuccessful,” she said.
Halt on redeterminations
There were two time periods — first for a few months in the beginning of 2015 and then again from November 2015 to March — when the OHA stopped making OHP members renew their membership into the program. Instead, when their renewal dates came, they simply remained on the program. That’s because OHA was in the midst of transitioning from Cover Oregon to a new enrollment system, said Dr. Varsha Chauhan, the OHA’s chief health systems officer.
As a result, the OHP population may have artificially ballooned during that time as more people were added while others remained on the program without needing to reestablish their eligibility.
Because of that, there are still things OHA doesn’t know, Chauhan said.
“Are they truly eligible? Are they people we’ve never put through the renewal cycle but are still getting benefits?” she said. “This is a good thing on one hand — anyone can debate it in any way — but the point is it’s a safety net for people.”
OHP assisters busy
Meanwhile, the places helping people sign up for OHP or renew their memberships say they’re slammed.
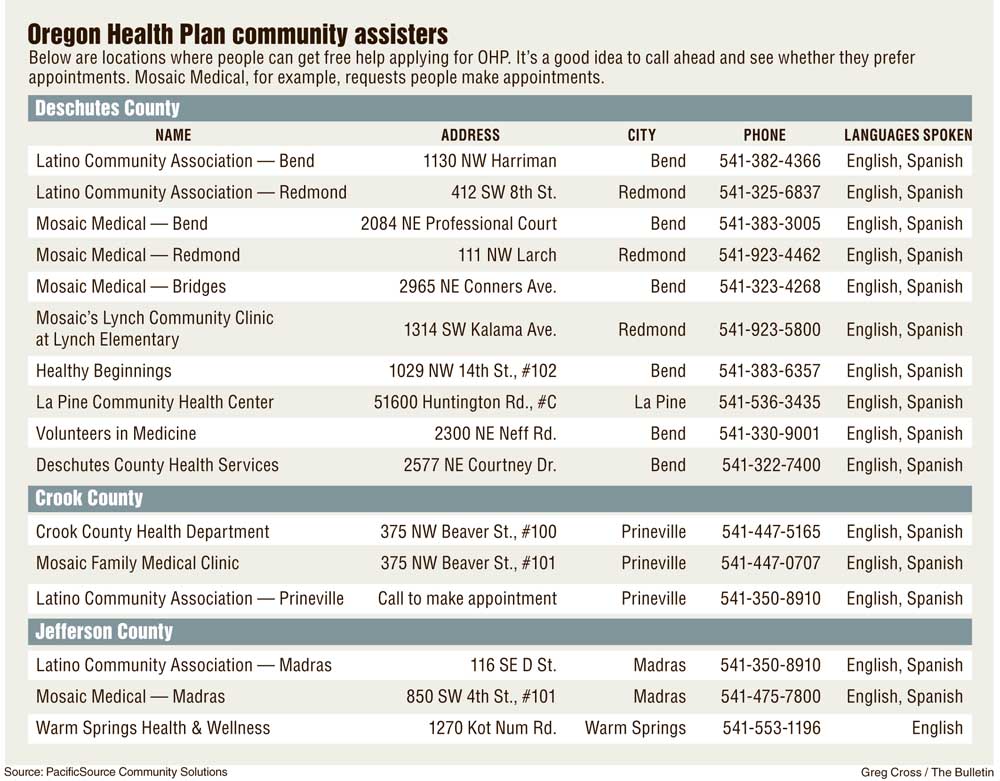
Mosaic Medical, a community health center, has seven people providing the free assistance in English and Spanish at six Central Oregon locations. Elaine Knobbs, Mosaic’s director of programs and development, said Mosaic asks that people call ahead and make appointments, which are currently being scheduled a week out, on average.
“It’s just a capacity issue,” she said. “It goes up and down so it’s really hard to staff for it.”
The Latino Community Association, a nonprofit that provides a variety of services, such as employment, legal and tax help, is also offering the OHP assistance at locations throughout Central Oregon. The association has helped 1,700 people with their enrollment or renewals over the past three years.
Martha Lina Romero, the association’s OHA enrollment specialist, said they’re “very, very busy.”
“I actually get to work and there is already a line,” she said. “A lot of people waiting.”
Once people lose their OHP coverage, there are indications it can take a while to enroll in the program again. Roughly 8,000 OHP applications have been waiting longer than 45 days, which is the federal time limit for the state to process the applications, said Wes Charley, OHA’s interim director of member services. Another 23,000 applications are being processed but haven’t surpassed the 45-day mark, he said. A single application can represent several people in a household.
Charley said he expects the OHA’s new enrollment system, called the ONE system, will speed up renewals and first-time enrollments because it features an online portal where, much like a bank account, people can update their contact information, make changes to their family composition and check their status.
“It’s a huge, huge improvement and we expect that to be the biggest impact for members as we move forward,” he said.
Currently, about 6,300 members are enrolled in the ONE system. Charley said he expects all members will have access to the system by March 2017.
While people wait for their OHP applications to be processed, they have to pay for any medical services they need out of pocket. They may be able to be reimbursed once they’re enrolled in OHP.
Farley, of PacificSource, said that can be difficult for people with chronic conditions who require maintenance medications, for example.
“I’m sure that break in coverage can definitely cause a problem,” she said.
— Reporter: 541-383-0304,
tbannow@bendbulletin.com








