Alcohol a top ER driver in Bend
Published 11:56 pm Friday, October 13, 2017
- Alcohol a top ER driver in Bend
Most festivals revolve around beer in Bend. Depending on the time of day, the unmistakable smell of brewing might permeate the air. Alcohol is a celebrated hallmark of Central Oregon culture. It’s also one of the most common reasons people end up in the emergency room.
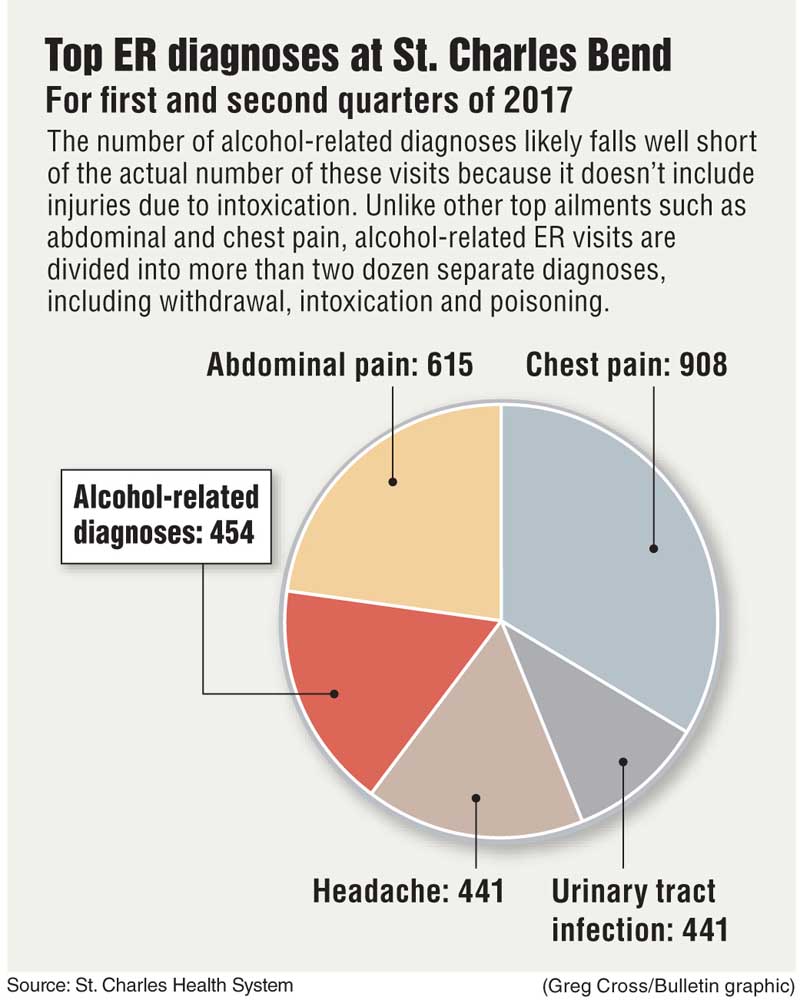
During the first half of this year, St. Charles Bend saw more than 450 emergency room visits where alcohol was the primary diagnosis. Most of those patients were going through withdrawal, intoxication and poisoning.
That number, while high, likely falls well short of the actual number of ER visits stemming from alcohol use. It doesn’t include the higher number of cases where alcohol is down the list as a secondary or tertiary diagnosis. And while it includes a small handful of cases of alcohol-induced liver failure and pancreatitis, it leaves out most of the serious health conditions exacerbated by drinking.
It also misses injuries that happened because the patient was drunk.
“That’s not counting the many, many people we see here that will leave with a diagnosis of sprained ankle or clavicle fracture or concussion,” said Michelle Brenholdt, the director of St. Charles Bend’s emergency services and trauma program. “They fell off the ladder because they were drunk, but it doesn’t get coded as alcohol.”
It’s not just here, either. Nationally, the rate of ER visits for alcohol-related diagnoses increased 38 percent between 2001 and 2010, according to the Centers for Disease Control and Prevention.
When people suspected of having a substance use disorder show up in St. Charles Bend’s ER, they’re met with a social worker who assesses them and refers them to the appropriate treatment program. But some treatment providers want to take that a step further. Rather than referring patients to a substance use counselor for a future appointment, they envision having that counselor right there in the hospital.
“I think there is a lot of interest in that right now and I bet within the next year we’ll have something like that going,” said Rick Treleaven, the executive director of Redmond-based BestCare Treatment Services, a drug and alcohol treatment provider.
Treleaven has been in talks with St. Charles about the program. Ideally, he said BestCare would employ the counselor, who would then work in the hospital. He or she would keep in touch with patients after they leave the hospital to ensure they make it to treatment and aren’t putting themselves in risky situations.
St. Charles is on board. Molly Wells-Darling, the health system’s director of inpatient behavioral health services, said it’s a great idea.
It’s one that St. Charles has considered itself, but the health system can’t afford to hire a counselor, she said.
“If that’s something they can make work, we would be happy to work with them,” Wells-Darling said. “They’ve always been a fabulous partner to work with.”
Allen Gibson, assistant program manager for Pfeifer & Associates, an alcohol and drug treatment provider with offices in Bend, Redmond and La Pine, said having a substance use counselor in the ER would be “extremely valuable.”
“When I heard BestCare was going to do that I thought it was an excellent idea,” he said. “I really, really hope they can pull it off and get something going.”
Social workers deal with a broad umbrella of patients and issues, including family problems and mental health disorders, Gibson said. With substance use counselors, there’s a higher level of expertise.
“It’s the same thing if you’re having cardiac problems,” he said. “I’m pretty sure you’d want to see a heart doctor.”
Further, having a counselor focused solely on substance use patients might mean those patients get more one-on-one attention, said Dr. Mike Franz, medical director of behavioral health for PacificSource Health Plans, which oversees care for Central Oregon’s Medicaid members.
Any amount of time would help. It’s a complex group of patients — battling not only addiction, but often mental and chronic physical health conditions on top of stressors like homelessness — and BestCare has made it a priority, Treleaven said.
“The level of health and mental health distress in this population is quite high,” Treleaven said. “It’s a difficult population.”
Many alcohol-related ER visits are among Central Oregon’s Medicaid patients. Roughly 15 percent of adults on Medicaid in Central Oregon have been diagnosed with a substance use disorder or a substance use disorder and a severe mental illness. That group comprises nearly 38 percent of emergency room visits among the region’s Medicaid population.
A study published last year in the journal Alcohol and Alcoholism showed that nationally, total alcohol-related hours spent in ERs increased from 5.6 million in 2001 to 11.6 million in 2011, an increase of 108.5 percent. Patients overall received more advanced imaging tests and had longer stays during that time, the study found.
Peter Mullins, a lead author on the study and a scholar with the George Washington University Center for Healthcare Innovation and Policy Research, said his team was surprised to see how long patients were spending in ERs for alcohol-related diagnoses.
He said having a substance use counselor in the ER is a great idea, and he hopes the program in Bend includes follow-up research to see whether it can be replicated elsewhere.
“Any more awareness and potential solutions that come down the pipeline for reducing that burden on the system is a really good thing,” said Mullins, a fourth-year medical student in George Washington University’s School of Medicine and Health Sciences.
St. Charles performs a standardized drug and alcohol use test on every ER patient called Screening, Brief Intervention, and Referral to Treatment (SBIRT), Brenholdt said. If they test positive, providers run a more in-depth screen and, if necessary, discuss options available to help them.
Research has shown SBIRT tends to work well when used in primary care, but not so much in ERs with patients who are intoxicated. A meta-analysis of 23 studies published in June in the Annals of Emergency Medicine was not able to identify a strong link between brief interventions in ERs and lower alcohol consumption later on.
Oftentimes, intoxicated patients just need a place to sleep it off. St. Charles will either keep those patients in the ER until they’re sober enough to leave or send them to BestCare, which runs a detox facility in Redmond, Brenholdt said.
Withdrawal from alcohol can be life threatening. Some patients can have seizures and require extensive medical support. Patients with alcohol poisoning might need a breathing tube or intravenous fluids.
“It can get quite complicated,” Brenholdt said. “They can be quite sick.”
—Reporter: 541-383-0304,
tbannow@bendbulletin.com
“That’s not counting the many, many people we see here that will leave with a diagnosis of sprained ankle or clavicle fracture or concussion. They fell off the ladder because they were drunk, but it doesn’t get coded as alcohol.”— Michelle Brenholdt, director of St. Charles Bend’s emergency services and trauma program






