Neurologists overwhelmed by stroke calls
Published 12:00 am Sunday, January 13, 2019
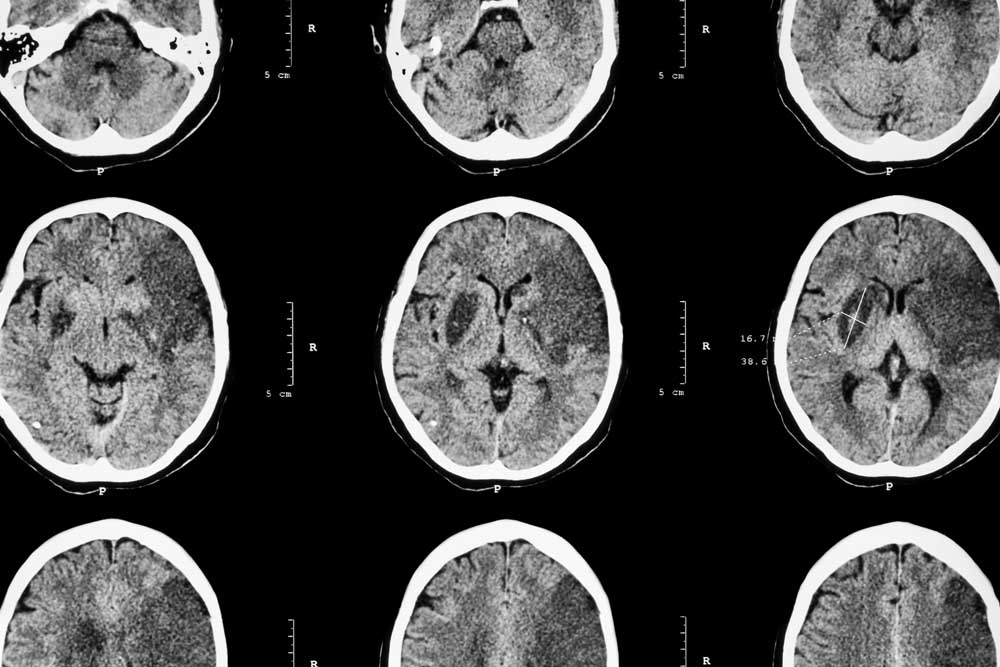
- This CT of a brain shows a cerebral infarction. (123rf)
An increased demand for stroke evaluations at St. Charles Bend has overwhelmed community neurologists, leading to an overhaul of stroke care at the hospital and the injection of new stroke care expertise.
The hospital has relied on neurologists in private practice to take turns being on call to evaluate patients arriving at the emergency with suspected strokes. With a growing and aging community as well as major advances in stroke treatment, the demand for such evaluations has grown exponentially in recent years. Neurologists found they were being pulled away from their scheduled patients to respond.
“You’re trying to get through a day of clinic on call and you would get 30 to 40 pages, and everything’s an urgency,” said Dr. Michael Bell, a neurologist with Bend Neurological Associates. “We couldn’t do both clinic and hospital medicine.”
Bell said of the three neurologists who have left practice in Bend in recent years, two cited the call burden as the reason.
“It’s been difficult to recruit and keep doctors,” he said. “Nobody can do this level of call and run a practice.”
Last year, the neurologists took their complaints to the hospital, which agreed to add new resources for stroke care. In November, St. Charles began using video consults with stroke specialists at Oregon Health & Science University to help evaluate patients.
“We’ve been doing that for two months, so stroke patients have access to not just a neurologist, but a neurologist with expertise in stroke at OHSU,” said Dr. Jeff Absalon, chief physician executive of the St. Charles Health System.
Hospital officials have signed a memorandum of understanding with the Portland-based academic medical center to bring neurologists to work full time at the Bend hospital.
The hospital expects to have two neurohospitalists — neurologists who practice solely in hospital settings — on board by mid-March, and could hire a third to provide round-the-clock, in-hospital coverage for neurology patients.
The increased demand for stroke care is due, in part, to medical advances, including the development of drugs that can break up clots causing strokes and retrieval techniques that allow neurosurgeons to remove clots by wire. Recent studies have expanded the window in which such techniques can be successful, expanding the number of patients who need a quick evaluation.
St. Charles has built a stroke program that now pulls in patients from much of Central and Eastern Oregon. With Bend’s population growing, particularly with an influx of retirees, the demand for stroke services has never been higher.
The region is undersupplied with neurologists as is, and new patients often have to wait weeks or months for an outpatient appointment. Many of the neurologists in private practice specialize in other aspects of neurology care. Bell is an epilepsy specialist, while his partner specializes in multiple sclerosis. Other neurologists in Bend are peripheral nerve specialists.
Stroke care, Bell said, is not in their wheelhouse.
“There was some tension about would neurology give up call if the hospital didn’t find some solution to this problem,” Bell said. “Now we’re going to have the best of both worlds. Instead of having some busy neurologist stuck in clinic trying over the phone to make an appropriate decision about a stroke, there will be a live neurologist in the day time at St. Charles.”
The community neurologists will continue to take emergency calls for other types of neurology patients.
The volume of stroke calls has been an issue for neurologists in many communities across the country. A recent survey by the American Academy of Neurology found that 41 percent of neurologists felt there was an insufficient workforce to handle stroke care, and 46 percent said stroke call duties were contributing to their personal feeling of burnout.
“Some programs do have stroke neurologists; some have neurologists that beam in, through telemedicine,” said Dr. Helmi Lutsep, a professor of neurology at OHSU and a co-author of a summary of the survey findings. “And some others, it really does fall all on the shoulders of the general neurologists in the community.”
As stroke care has become more complex, many community neurologists feel less comfortable taking stroke calls, uncertain whether they’re up to speed on the latest developments in stroke diagnosis and treatment.
“I get lots of calls from general neurologists, because they’re just not familiar with stroke care,” Lutsep said. “It keeps changing, so i think that there’s a fear component that you’re always one step behind potentially.”
Stroke outcomes are incredibly time sensitive, and many regional and local hospitals are adopting telemedicine to cut down the time. Such services have doctors available immediately at all hours, eliminating the need to rouse doctors in the middle of the night and wait for them to arrive at the emergency room.
“We’ve been working on things like how we make sure we identify patients as early as possible, and how do we make sure that patients present for care as early as possible,” Absalon said. “The earlier the care, the better your outcomes are.”
— Reporter: 541-633-2162, mhawryluk@bendbulletin.com






