Editorial: Don’t stop surgeries in the middle because of insurance
Published 8:37 am Saturday, April 26, 2025
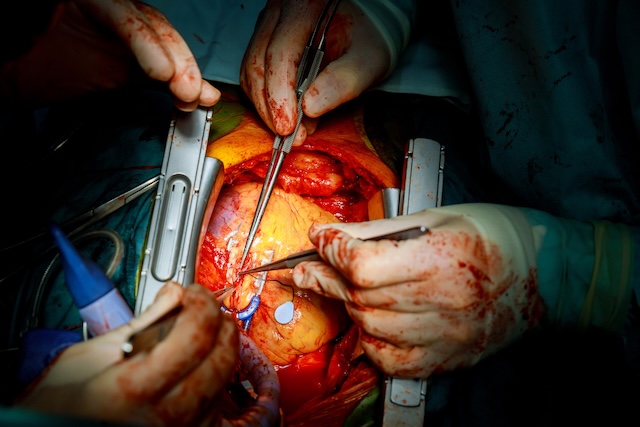
Surgeons will sometimes stop in the middle of a surgery when they see something that may require prior authorization from a patient’s insurer and they don’t have the authorization to take action.
It sounds odd. It doesn’t happen often. It can be for the patient’s benefit to ensure what is going to be done is covered by insurance.
State Rep. Rob Nosse, D-Portland, told a legislative committee this week about his bill, House Bill 3134, that would change that scenario. The bill, as it is proposed to be amended, prohibits insurers from requiring additional prior authorization for additional or related procedures identified during surgery if delay wouldn’t be medically wise, any additional procedure would be covered and the additional procedure is not experimental or investigational.
It’s a complicated bill. It was first opposed and then endorsed by some providers. Insurers came out against it.
The idea behind the bill is right. Medical professionals should be the ones who are deciding the best course of action when something unexpected comes up during surgery, not concerns about insurance. But it was sure hard for us, at least, to tell during a committee hearing Wednesday if legislators have got this bill right.