Is pain all in your head?
Published 12:45 pm Tuesday, July 24, 2018
- Is pain all in your head?
{%comp-FFFFFE-tl%}
Health problems always seemed to be more drastic for Bill More than for others. He wouldn’t just get a cold — he’d get bronchitis. While other kids were skinning knees or bruising elbows, he was breaking bones. But for most of his life, the Bend man was in great physical shape. He took up snowboarding in the 1980s and raced with the U.S. Ski and Snowboard Team. Then about six years ago, when he was 36, a car accident changed the course of his life.
He hurt his back and couldn’t seem to get over his injuries. Pain radiated from his lower back down to his foot. Unable to exercise or even work, he lost 20 pounds of muscle.
“I just could not recover from it,” he said.
The injury sent More on a medical odyssey. He jumped from doctor to doctor and tried procedure after procedure in a fruitless attempt to quell his pain. He put together a binder — now 6 inches thick — chronicling his journey through the health system: a discectomy to relieve nerve pressure in his back, a fusion of his sacroiliac joint, injections, stem cell treatments, another discectomy.
“I just went from one doctor to another,” he said. “There’s gotta be something somebody can do, or give me an answer about why I feel like this all the time.”
His doctors were out of ideas. “You’re just going to have to learn to live with it,” he recalls them saying.
“You get home and you haven’t slept for four days. You’re just writhing around night after night.”
None of his medical treatments were helping. Desperate and in constant pain despite being on massive doses of opiate drugs, More and his wife began preparing for his death.
Pain may be the most universal human sensation, having evolved as a way to protect the body against potential dangers. From our first days of life, we feel pain and quickly learn to avoid the things that cause it. Over the ensuing years, our experiences firmly ingrain the notion that damage to our body causes pain, and when the injury heals, the pain fades away.
This construct, however, is based on an illusion of how pain — and particularly chronic pain — actually works.
There’s an emerging understanding among pain specialists and researchers that the brain doesn’t sense pain so much as it produces it, and that the sensation of pain is heavily dependent on the psychological and social stressors in a person’s life. Moreover, when that system goes awry, seemingly innocent sensations can get amplified and reinforced, potentially resulting in a lifetime of pain and affliction.
This disconnect leaves chronic pain patients searching for an answer to their suffering, trying surgeries, injections and painkillers that have little chance of addressing the true cause of their pain but leave them at risk for complications and early death.
“The old way of understanding pain assumes that the pain that you’re experiencing has a direct relationship to something bad that’s happening in your body where you’re feeling the pain,” said Nora Stern, a physical therapist with Providence Health in Portland and a member of Oregon’s Pain Management Commission. “When you’ve been living with pain for long time, that whole process becomes a lot more complicated and becomes involved with the amount of the difficulties that people are having in their lives.”
Not all types of chronic pain are caused by this haywire reaction in the brain. Certainly many patients have injuries that haven’t healed or an ongoing disease with painful symptoms. Others develop damage to their nerves or the nervous system that creates ongoing pain. But the vast majority of patients living for years with recurrent pain have none of that.
“We can’t identify any disease. There’s no infectious agent; there’s nothing that’s broken; there’s no nerve cell receptor that we can find that’s abnormal,” said Dr. David Sibell, a pain specialist with Oregon Health & Science University’s Comprehensive Pain Center in Portland. “But the nervous system reacts in an enhanced way to stimuli, such that normal stimuli become painful and moderately painful stimuli become even more painful.”
{%pl-6226625%}
As patients seek a physical explanation for their pain, X-rays and MRIs lead to procedures and surgeries, none of which provide much relief. It’s this disconnect between physical damage and pain that underlies much of the futile treatment and duplicative care in the health system today.
All in your head
More went from doctor to doctor seeking a cure, which he believes just reinforced the idea in their minds that he was exaggerating or inventing his pain. Chronic pain patients, who often have no visible defects or injuries, are regularly met with skepticism rather sympathy, forced to justify themselves to a society that doesn’t understand pain or expects people to muddle through it.
“People don’t know why we might be a little short or why we’re parking in a handicapped parking spot,” he said. “You have no idea the amount of pain it takes to walk into the grocery store some days.”
Soon, More began doubting himself.
“You start to think maybe it is in my head and maybe I am crazy,” he said. “People start thinking you’re exaggerating everything and so you just learn to keep it to yourself.”
Pain experts like Dr. Lorimer Moseley, a professor of clinical neurosciences at the University of South Australia, maintain that pain is all in the patient’s head, although not in the way you might think.
“The brain does not recognize pain coming from something else,” Moseley said during a recent presentation at the university. “The brain produces pain.”
Let’s say you step on a sharp object with bare feet. Danger receptors, known as nociceptors, sense that object and send an electrical signal to the spinal cord. The spinal cord then sends that signal up the brain, which must then determine whether there’s a potential danger. The brain makes use of sensory inputs and memory to put the signal into some context and determine how much of a danger it represents, then sends a warning signal back down to the foot in the form of pain.
“We feel pain in our body, and we feel it at a particular location,” Moseley said. “But it is impossible to feel pain without a brain, and it is completely possible to feel pain without the body part.”
That may sound crazy, but consider that individuals who lose an arm or a leg often feel sensations in that limb even after it’s gone. Phantom limb pain affects up to 80 percent of amputees and can be mind-numbingly difficult to relieve. Imagine feeling an itch on your ankle that you can not scratch and or a cramp that you can’t stretch out.
Doctors have developed techniques to address phantom pain that often rely on fooling the brain that the limb still exists. Dr. Vilayanur Ramachandran, a neurologist at the University of California, San Diego, developed mirror therapy to do just that. He had patients with amputated legs watch a reflected image of their intact foot in a mirror as they tried moving both feet simultaneously. When the brain was fooled into thinking that both legs were moving, the pain in the phantom limb dissipated.
Moseley argues that all pain may in fact be phantom pain, not in the sense that it isn’t real, but that the brain projects pain onto the part of the body it is trying to protect. It’s much like the concept of vision. The image we see isn’t out in front of us, it’s in our brains, and as such we are easily fooled when what we see and what the brain thinks we are seeing don’t line up.
“In reality, cognitive neuroscientists conclude that all perceptual experience is produced by your brain,” Moseley said. “And pain is no exception to that.”
His research team has found many variables can change how much something hurts, underscoring the disconnect between tissue damage and pain.
{%tr-F5E5CC, 000000, 2%}
“Your pain depends on how much danger your brain thinks you’re in, not how much danger you are really in,” Moseley said.
His most famous experiment to prove the point was one he came across naturally and described in a widely viewed TED Talk video. Years ago, he was walking through the Australian bush when he felt a tiny prick or scratch on the outside of his left leg. It was a sensation he’d felt plenty of times before, and so when the brain received the danger signal, it was discounted as not much of a threat. He felt no pain and calmly continued on for a swim. He woke up in a hospital four days later having survived a bite from an eastern brown snake, the second most venomous land snake in the world.
Nine months later, he was back in the bush and he again felt something scratch the outside of his left leg. He felt “a white hot poker pain screaming up” his entire leg. As he looked to see how bad the snake bite was, he saw it was actually just a tiny scratch from a little twig.
“My brain said, ‘This is very dangerous’ and I had severe pain and the location of my pain was in exactly the right place,” he said. “And intriguingly, not only at the scratch but my whole leg was burning and it was intense.”
Researchers believe the brain uses the information at its disposal to evaluate the danger to the body and protect it with a corresponding amount of pain. In chronic pain patients, the brain has learned to treat seemingly innocuous dangers as potentially catastrophic.
“It’s as simple and as difficult as this: Anything that changes your brain’s evaluation of danger will change your pain,” Moseley said. “So if you are in pain, you’ve got some really tough questions to ask yourself. What in my life … implies that I am in danger?”
The opioid system
Pain researchers recognized the connection with danger or stress decades ago in soldiers who in the heat of battle would feel no pain despite enduring horrific injuries. Eventually, they realized that pain was a two-way street with signals rising from the site of the injury up to the brain, and signals coming back down from the brain, all of which was mediated by a set of neurotransmitters that pain scientists call the body’s natural opioid system.
“The way we began to think about stress-induced analgesia, the top-down effect, is so closely linked to the opioid system, they can’t be separated,” Dr. Jane Ballantyne, a pain medicine specialist at the University of Washington said at a pain conference in Oregon last year. “The opioid system is our pain system. It is the way we defend ourselves.”
Opioids are a class of drugs made from the poppy plant or synthesized to create the same effect. Natural versions include drugs like opium, heroin and morphine. Synthetic versions, such as Vicodin, Percocet or Oxycontin, are among the most potent pain relievers.
But the body also produces its own opioid-like chemicals, called endorphins, enkephalins and dynorphins, which function as neurotransmitters. Those natural opiates are released during times of stress as part of the fight or flight response to counteract pain. So a lion that injures its paw in the middle of a hunt can continue chasing its prey when the flood of opiates blocks its pain. But researchers also discovered that natural opioids have a dual function: They can promote pain just as easily as they can block it.
“When the lion is injured and resting, as long as you don’t go near the injured paw, it’s not painful,” Ballantyne said. “The moment you touch it, it’s hypersensitive.”
It’s this hypersensitivity that researchers believe is at the heart of chronic pain. Ballantyne explains that an injury prompts electrical signals that are sent to the brain, causing a release of chemicals and a neuroinflammatory process in the brain. Brain cells die and the brain remodels itself. When that process continues repeatedly, it can become ingrained and the central nervous system gets sensitized to feel pain even in the absence of tissue damage or injury.
“All of this goes to explain why some people have such profound changes in the brain after injury, that those changes don’t reverse, even if the injury improves,” she said. “We don’t really understand why in some people it gets perpetuated or you get this central sensitization to make sure it never goes away.”
The constant reactivation of the body’s natural opioid system can create a state of hypersensitivity that responds to the slightest provocation with pain. The problem ceases to be the knee or back or whatever other injury first precipitated the pain. It’s now become a malfunction of the pain system, or as Dr. Daniel Clauw, a pain expert with the University of Michigan, calls it, brain pain.
{%qc-“This really is a big fundamental change in how we think of chronic pain. In some individuals we need to treat the amplifier setting, not what’s going on in the periphery.” %em Dr. Daniel Clauw, a pain expert with the University of Michigan%}
To explain it to patients, Clauw likes to use the analogy of an electric guitar and amplifier. The volume of the sound doesn’t depend so much on what’s going on with the guitar as with the setting on the amplifier. In people with central sensitization, the dial on their amp has been turned way up. So sensory inputs that wouldn’t normally have much impact result in significant pain.
“This really is a big fundamental change in how we think of chronic pain,” he said. “In some individuals we need to treat the amplifier setting, not what’s going on in the periphery.”
Pain doctors now consider chronic pain as a malfunctioning of the pain system, where the brain, the spinal cord and the nerves that go down into the body, aren’t functioning in the way they should be.
Scott Safford, a pain psychologist with St. Charles Health System in Bend, likens it to a car alarm that continually goes off for no reason or is triggered by the slightest vibration of a passing car. “It doesn’t mean that somebody’s car is being broken into,” he said. “I sort of conceptualize chronic pain in a similar way. The pain signaling system is saying, ‘There’s something wrong, there’s something wrong,’ but it doesn’t necessarily mean there is something at a musculoskeletal level that’s wrong.”
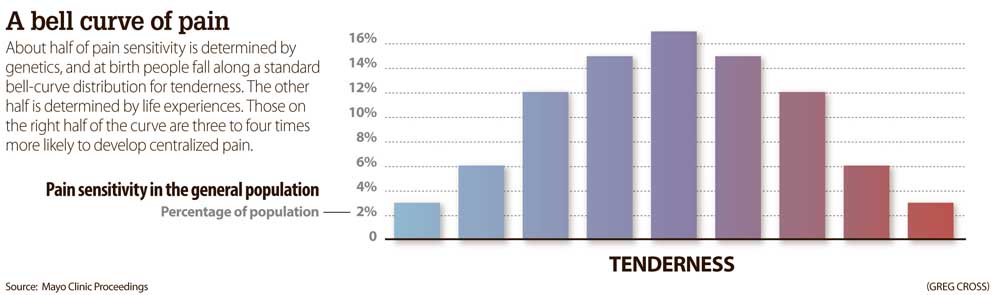
Why such sensitization happens in some people and not others is still a mystery. But there are some clues. Clauw said that people are born with different levels of pain sensitivity that can be plotted on a standard bell-shaped curve.
“About 50 percent of how tender you are, or what your volume control is, is determined by the genes that you are born with, and 50 percent are things that happen to you after you are born,” he said. “The people on the right side of this bell-shaped curve are three to four times more likely to develop chronic pain than the people on the left.”
Those born at the right side of the curve often start developing different types of chronic pain early in life. They experience growing pains as children, and then develop headaches or painful menstrual periods in their teens. In their 20s, they have low back pain, irritable bowel syndrome or painful bladder syndrome. Eventually, their pain becomes so widespread they get diagnosed with fibromyalgia, which Clauw calls the poster child for centralized brain pain.
“Fibromyalgia was really the first condition that was generally recognized where the pain couldn’t possibly be due to the damage or inflammation in the peripheral tissues because people hurt everywhere,” he said. “All their labs are normal, all their X-rays are normal, everything is normal. Literally it’s at the end of this continuum of centralized pain, but it’s really taught us about everything in between.”
A diagnosis
After several years of seeking a treatment for his pain, unable to work and unable to snowboard, More began to descend into despair.
“Everything had gotten so weak, it was hard to get out of bed most days. I hit rock bottom,” he said. “There was nothing directly threatening my life, but you can only take so much. If I wasn’t able to rein it in a little bit from where it was, I couldn’t imagine managing that amount of pain for more than another couple of years.”
More thought about writing a letter to his doctor and hiding it in his bedroom. “If I happen to die from something you prescribe, it’s because I wanted to. It’s not on you.”
Dr. Philip Wallace, a physical medicine and rehabilitation specialist with Northwest Brain & Spine, was one of the few doctors who never seemed to doubt More’s pain. There were days when they would spend an hourlong appointment just talking about options, and tearing up.
Then one day two years ago, More was sitting in an appointment room with sunlight shining directly onto his face, when Wallace noticed something unusual: a blue tint in the whites of his eyes. It could mean only one thing. More had a condition known as Ehlers-Danlos Syndrome, a disorder of the connective tissues in the body.
{%pc-6299484%}
Caused by a genetic mutation, the syndrome, commonly referred to as EDS, causes a lack of collagen that leads to loose joints, stretchy skin and fragile tissue. The lack of collagen in the eye results in a characteristic blue tint. The condition, which may affect as many as 1 in 5,000 individuals, is little known and commonly overlooked.
The diagnosis explained why More incurred such severe injuries. With super-loose joints, he could dislocate his shoulder by turning a doorknob or even by waving hello. His ribs would regularly pop out of place. “It doesn’t mean there’s a cure or anything, but at least I can put a name to it,” he said. “That alone is a huge relief.”
It also explained why More had such trouble getting past his injuries and back pain. EDS has one of the highest rates of centralized pain among chronic pain conditions.
“We’re really not sure why,” Clauw said. “The leading theory is that — just like the higher rates in other chronic pain states — that ongoing nociceptive pain can cause pain to centralize in many people.”
EDS falls in the same high range as sickle cell disease. Those with either condition often have lifelong histories of acute pain that lead to central sensitization.
Once researchers understood that pain is a product of the brain, it helped to explain how someone’s psychological and social state influences his or her pain. Over time, they came to believe that thoughts and emotions may play a larger role in pain than any tissue damage or injury.
“Often the roots of the pain are much, much, much deeper than what’s going on physically,” Ballantyne said. “These roots are created by past experiences, by present fears, something terrible is going on, and it may not be explained by pathology and found at all in the body.”
The role of childhood trauma is particularly strong. By some estimates, up to 30 percent of chronic pain patients have experienced sexual abuse, and more have undergone some sort of physical or emotional abuse. Patients who end up seeking help at pain clinics are those who simply cannot throw off the stresses of life and develop chronic pain instead.
“I would say that 90 percent of my patients have had some trauma,” said Allison Suran, a physical therapist with Healing Bridge in Bend. “If you have a brain that’s already been trained to be hyperalert for your safety and survival, and then something seems threatening, it will interpret that as more threatening.”
Modern science is now allowing pain researchers to measure this effect of stress and emotion on pain, using tools such as functional MRI to see what parts of the brain were being activated. Researchers from Northwestern University recently showed that when pain becomes chronic, it activates an increasingly larger part of the brain, until the pain response starts to overlap with the emotional and reward centers of the brain.
{%tr-F5E5CC, 000000, 3%}
Studies with laboratory rats have shown that pain is moderated by two types of pathways, one that inhibits pain and one that facilitates it, and that both can be activated either by external painful stimuli or the individual’s state of mind.
Dr. Howard Fields, director of the Wheeler Center for the Neurobiology of Addiction at the University of San Francisco, showed that when rats are placed in a cage with a predator, their brains are flooded with natural opiates, turning off the pathways that promote pain and turning on the pathways that inhibit it. Giving rats an opioid drug like morphine produced the same effect.
Opioids, whether produced by the brain or taken as medication, he found, could either worsen or relieve pain depending on the individual’s emotional state.
“The problem is that when we give exogenous opioids, we overwhelm these systems,” Ballantyne said. “They’re the natural systems that help us deal with pain. But once we commandeer that whole system … we’re sort of not allowing that system to work for us.”
When patients are treated with very high doses of opiates after a surgery, for example, it changes their natural balance between pain relief and sensitivity to pain. But when patients stop taking those drugs, the balance does not revert to its original levels.
Patients end up developing a tolerance to the drugs.
Moreover, the longer the patient takes the medication, the greater the imbalance, and the patient will need higher levels of external opioids to restore their balance. They become dependent on the external opioids, and if they don’t get them, they begin to exhibit symptoms of withdrawal.
The pain treatment field has largely come to the conclusion that opioid medications make chronic pain worse, exacerbating the hypersensitivity of the pain system, leaving patients in worse pain than they had before starting the medications. Patients and their doctors often mistake this escalation of pain as a worsening of their systems, leading to an increase in their prescribed dose. But if they try to reduce the dose, they wind up feeling symptoms of withdrawal, which in turn they misattribute to an underlying health problem.
“Some of these patients may truly believe that opioids are helping them,” said Dr. Andrew Kolodny, executive director of Physicians for Responsible Opioid Prescribing. “I’m not sure the opioids are. I think the opioids are treating their withdrawal pain.”
This effect has been measured with laboratory mice as well. Scientists have done experiments in which they place a mouse’s tail on a hot plate and then slowly turn up the temperature to see how hot it gets before the mouse feels pain and flicks its tail off the hot plate. When mice are given opioids, they tend to flick their tails off at much lower temperatures. The opioids lower their pain threshold. Their pain gets worse.
In some patients, the pain medications may help to reduce the pain of their initial injury but wind up making their overall pain situation worse.
“Let’s say they have lower back pain and maybe it makes that 30 percent better. But then they develop pain all over their body,” Sibell said. “It’s an unfortunate side effect, but some people develop this hypersensitivity, and actually have reduced function and increased pain overall.”
Sibell said that despite a worsening of their condition, patients are reluctant to give up on pain medications and medical procedures in part because that’s been the promise of medicine for hundreds of years, that doctors can fix what’s broken, can address what’s wrong and restore the patient to their original state.
{%pr-6228658%}
“The metaphor that a lot of people use is, you can’t unboil an egg,” he said. “There are some conditions that you can’t fix.”
But the hope of a fix, the dream of being pain-free, is a seductive one, and one that patients aren’t willing to give up easily. Sibell had one patient who was scheduled to have his 14th back surgery. Each of his prior 13 surgeries had made his situation worse.
“Well, I have hope for this one,” he told the doctor.
“For someone who is basically living in a state of suspended animation, there is no reality check,” Sibell said.
He saw another patient who was taking 13,000 milligrams of Tylenol per day, a massive dose that put him at severe risk for liver failure. When the patient admitted it wasn’t really helping him, Sibell asked him why he continued.
“Because you have to do something,” he replied.
A conscious decision
Once More had his diagnosis, his life changed dramatically. He had been on opioids for two to three years but was becoming increasingly concerned about what they were doing to him.
“I don’t know if I would have survived without them. The only other option was death or find heroin or something, because it was that bad,” he said. “But I got to the point where it’s had a big effect on my brain, it just starts making you go insane. You just can’t imagine another day like that. You just want your days to get shorter and shorter, because you just can’t break the pain.”
Convinced the drugs were no longer helping him, More decided to quit cold turkey.
“I think everybody gets to the point where they are not effective and you’ve got to make a personal decision,” he said. “Are you going deeper into the opioid hole? The only other way I figured I was going to survive the pain was by making my brain stronger, strong enough that I can handle this.”
The opioids were a backup plan, a crutch that he knew he had to discard or he would wind up using.
“I went through hell a few months ago. It was like heroin withdrawal,” he said. “I didn’t expect it. It was a few weeks of just misery to do it, but I just needed to do it. There was no point in taking something that wasn’t helping any more.”
Many chronic pain patients simply can’t come to grips with the notion that their opioids might be making them worse or to conceive of giving them up. Patients often say that medication is the only tool they have to manage their pain.
“There’s a communication challenge, because opioids make your patient happy on the way home from the office and there’s no other chronic pain treatment that does that,” said Dr. Mark Sullivan, a pain specialist with the University of Washington. “Patients who say they’re doing great or surviving on meds if you look at them, most of them, they are not doing great. Population surveys show they are still having high pain levels, high levels of depression, high levels of disability. It’s not by any means a panacea.”
Sullivan and his colleagues at the University of Washington recently published a small study in The Journal of Pain showing that patients who underwent a support program to help them taper off of their drugs wound up with less pain and were less likely to have pain interfere with their lives. They had a lower risk of losing interest in their usual activities, having trouble concentrating or feeling down or sluggish.
“I think pain patients tend to overvalue their experience of starting and stopping opioids,” Sullivan said. “When they start, they feel better and when they stop they feel worse. In the middle, they’re not doing very well. But that gets discounted in the face of the kind of initial pain relief and withdrawal experiences in the end.”
Patients remember how great it felt when they started taking opiates and are always seeking that feeling again. But when asked if their pain level or functional status is any better after being on opioids for months, most say it is not. With long-term opioid use, the patient’s condition begins to look more and more like fibromyalgia — everything hurts.
Clauw estimates that only 20 percent of chronic pain patients may be getting any benefit from taking opioids. The rest are exposing themselves to major risks and may be making their condition worse.
{%pl-6299483%}
“The concern that a lot of us have is that a lot of people that have chronic pain are not taking opioids because of their analgesic effect. They’re taking opioids because for that 20 or 30 minutes when that opioid kicks in, your life doesn’t suck as much,” Clauw said. “It’s more of an antidepressant and antianxiety drug. If that’s why you’re taking opioids, we have better drugs with way less side effects to do that, and we have a lot of non-drug therapies that can do that as well.”
Many of the drugs that are now used to treat the brain pain in chronic pain patients have come out the fibromyalgia world. Antidepressants like Cymbalta (duloxetine) or Elavil (amitriptyline), and muscle relaxants like Flexeril (cyclobenzaprine) work by affecting those top-down natural opioid pathways that can minimize centralized pain. Neurontin (gabapentin) and Lyrica (pregabalin) were originally approved to treat certain types of epilepsy and nerve pain but are now commonly used to treat fibromyalgia as well.
And doctors have found that when patients respond to those drugs, they usually see multiple symptoms improve, whether that be insomnia, depression, anxiety or pain.
Studies showing that Cymbalta worked for peripheral nerve conditions such as low back pain and osteoarthritis were a watershed moment for the chronic pain field, showing just how big a role the volume control aspect played in chronic pain.
Buying in
In 2003, Michelle Marikos fell off a two-story porch at a party in Chico, California, pushed over the edge by a drunk sorority sister. With three crushed vertebrae in her neck, she came within a fraction of a millimeter from paralysis if not death. She spent the next six months at her home in Ashland in a brace to immobilize her head. Unable to get her pain under control, doctors prescribed pain relievers, anti-inflammatories, muscle relaxants, escalating her dose time and time again.
“You work up into this whole pillbox of all these pills,” she said. “It was pretty much just all the time in constant pain, whether you took the pain pills or not.”
Like More, she went through surgery, injections, nerve blocks, alternative therapies — anything to try to get her life back. “There was this whole host of things you get into with so many doctors looking for answers. I’ve got to get out of this pain, I cannot be like this. This is not who I’m supposed to be. This is not the life I’m supposed to live.”
She wanted to have a second surgery on her neck, but doctors said they couldn’t do the surgery unless she reduced her daily dose of pain medications. She enrolled in a six-week chronic pain management program at the Mayo Clinic in Rochester, Minnesota, that would help her taper off the opioid drugs.
{%tr-F5E5CC, 000000, 4%}
“I was the girl in the corner, just crying, for two weeks straight,” she recalled. “I couldn’t think what my life would be like. The fear was just overwhelming. I cannot live without these pain medications. It’s like a monkey on your back, where the monkey is telling you, you have to have these things, there’s no other way out.”
But after two weeks of tapering, she realized things hadn’t gotten any worse. Before the class was over, she had already decided she didn’t need the surgery after all.
“If I was going to taper off these medications, I was not going to have the surgery, and go back on,” she said. “That was not something I wanted to go through again.
Marikos learned techniques to help manage her pain, avoiding the boom-and-bust cycle that chronic pain patients often fall into. They overexert themselves when they are feeling good, causing a flare-up of their symptoms and putting themselves out of commission for days. When they recover, they feel the need to catch up on everything they’ve put off, restarting the cycle. Marikos learned how to pace herself, how to work efficiently in her orchard and how to take responsibility for her own pain.
“That was another aha moment of acceptance. This is your life and it’s OK to live with pain,” she said. “But it’s not OK to struggle and just survive. You have to be able to live.”
Now she counsels other patients with chronic pain, helping them break their own cycle of dependence on medications. She tries to sell them on the notion that their road to a better life might start with abandoning opioids.
“It’s a horrific sell,” she said. “You are so programmed to take that pill and feel one or two clicks better and that’s where you’re going to be.”
But once patients understand the pain medication is actually making their pain worse, the decision gets much easier.
“Getting off opioids and getting off all those medications, it’s not going to cure you. I’m not going to ever live without pain,” Marikos said. “But I’m going to live with less pain than I did with the medications. So why would I take the medication and walk around like a zombie, and feel like a nutcase all the time?”
Many providers ask patients to sign pain contracts to continue receiving opioids, and those pacts often require patients to try physical therapy or pain management classes. If patients see that alternative pain management strategies can work, they might be more amenable to tapering off their drugs.
“I have some patients that are coming into pain school and they are mad, because they don’t see self-management as a part of their care,” said Kim Swanson, a pain psychologist with St. Charles Health System in Redmond. “They see that having to participate in class is a barrier to getting the real treatment, which is the pill.”
But she’s also had many patients ask if they can attend the class again. Safford, who runs the pain classes in Bend, said most patients who attend want to learn better techniques for managing their pain and would rather be off of their pain medications.
“These people have had chronic pain for years and most of them have had negative experiences with health care providers,” Safford said. “Is their pain real? Is it not? Is it in their head? Are they drug seeking? So they already have a preconceived defensiveness about it.”
Many chronic pain patients have a long list of experiences where doctors, family and friends have doubted their pain. Doctors will tell patients they have good news, the results of the X-ray or MRI shows everything is normal.
“And those patients will walk away feeling like they’re crazy or the pain is all in their head,” Swanson said. “Whereas the language should really be rephrased to say, ‘I know you hurt. The good news is I don’t see any injury there. It doesn’t mean that the pain isn’t real but that something has happened in the nervous system that we just can’t detect.”
For many, the suggestion they should cut back on or stop taking opiates sounds like people don’t believe their suffering is real.
“Unfortunately what we’ve done is we created this concept of legitimate pain,” said Laura Heesacker, a licensed clinical social worker from Ashland. “If I were to say, you don’t have legitimate pain, what does that leave you with? Illegitimate pain. And how does that feel?”
Heesacker has been working with providers throughout the state on how to approach their chronic pain patients.
“They have to start with validating,” she said. “They can’t start with, ‘Oh, well you have brain pain and therefore there’s nothing I can do. You should go talk to a psychologist.’”
{%pc-6228730%}
Chronic pain patients are so used to having their pain discounted, they often feel the need to exaggerate their pain to ensure doctors won’t ignore it. When asked to rate their pain on a scale of 1 to 10, where 10 is the worst pain imaginable, patients sitting calmly in a chair rate it as an 11.
“They’re saying, ‘Please validate me,’” Heesacker said.
She’s sat in on many appointments where providers have told their chronic pain patients they want them to taper off their drugs. In that moment, patients often freak out, she said, reacting as if a Band-Aid is being ripped off of their pain.
“If they can, in that moment, reframe that patient’s behavior and understand that that is a survival skill, and that the patient is likely to do anything: sob, scream, threaten, be hostile. If the provider can stay calm and stay connected, and believe in their patient’s ability to make the change and to have confidence in themselves in working with this patient through this taper, that goes a long way,” Heesacker said. “Because these patients at that time, they don’t have that belief.”
It’s incumbent on the doctors, she said, to believe in their patients and help them understand that they’re not being pawned off on some subpar treatment because they have illegitimate pain.
{%tl-F5E5CC, 000000, 5%}
That’s another way that chronic pain differs from acute pain. Understanding the process is a crucial component of the solution. You can understand why a torn ligament in your knee causes pain, but it still requires a physical procedure to fix it. With chronic pain, understanding the process helps to interrupt the cycle. The patient who understands this is affected by worry and anxiety, can then take the steps to calm it.
Moseley’s group in Australia has conducted randomized clinical trials that show chronic pain patients who understand the notion of brain pain sleep better, worry less, have less pain and are more likely to be employed full time.
Small steps
Brock Monger, a physical therapist with Apex Physical Therapy in Madras, has seen many patients come through his door skeptical that physical therapy will help. They’re there only because it’s a required component of their pain contract. Others are scared that any little movement will leave them hurting.
Monger seeks to discover what those patients really miss doing in their lives and to find a way to get them moving toward that goal, both literally and figuratively.
“The whole thing of ‘no pain, no gain’ that does not apply particularly for patients with chronic pain because that’s a great way to ensure they don’t ever come back,” he said. “We know that movement can be a very effective modality, and I believe in ‘movement is medicine.’”
{%tr-F5E5CC, 000000, 6%}
To help clients get moving, he works with them at the pool, where every gallon of water that someone displaces takes 8 pounds of weight off their achy joints. The pressure of the water provides a steady, calming compression on their muscles, helping to modulate the pain signals coming to their brains. There’s an ease of movement in the water, yet more resistance. Clients are conditioning their muscles, but it still feels effortless.
“It’s really empowering to get someone in the water that can’t weight-bear on a painful limb, and see them be able to just stand upright in waist-high water,” he said. “It’s pretty empowering to see them happy with that.”
Angela Cruse has been dealing with pain for more than 30 years. A fall in the shower in 1984 led to a diagnosis of a slipped disc and put her in traction, with two 100-pound weights pulling on her body in an attempt to realign her spine. In 1996, she slipped on a wet landing at work and woke one morning several months later unable to feel her legs. Two years later a file cabinet tipped over on her, breaking her back. To treat her pain, doctors implanted a morphine pump and prescribed her Percocet and Valium. She used a walker or cane to get around. When she left California two years ago, she was taking eight 325-milligram Percocets per day. But the opiates left her groggy and unable to play with her grandkids.
“I didn’t like the way they made me feel,” she said. “I’d been trying to get off of them for years.”
In Madras, her new doctors were concerned about how many medications she was taking. They lowered the dose on her morphine pump and sent to her to physical therapy at Apex. Cruse had benefited from pool therapy in California, so she eagerly resumed pool work with help from Monger.
She’s now down to only 20 Percocet a month, using the medication only for breakthrough pain. It’s allowed her to get back to gardening. She’s adopted her 16-year-old granddaughter and enjoys throwing the football with her 8-year-old grandson. “I have my cane,” Cruse said. “But I hardly ever use it.”
Not all patients will be able to completely eliminate use of opioids. The goal of physical therapy and pain management programs is to reduce dependence and improve quality of life.
“I rarely ever tell patients, my goal is to get you off of pain meds,” Monger said. “If we can improve function, then oftentimes pain can decrease.”
For patients who go through the process and come out the other side taking fewer or no medications, the transformation can be extraordinary. They emerge from the cognitive fog that has been clouding their lives.
“That’s what opiates do,” Ballantyne said. “They don’t just kill the pain they also kill the pleasure. You have no enjoyment because emotionally you’re not able to experience life fully if you’re on opiates. And what they always say, ‘I’ve got my life back’ or ‘I’ve got my husband back.’”
More first visited Suran shortly after stopping his medications, and learned from her some of the techniques for quieting pain used in an approach called Feldenkrais. It involves gentle movements and directed awareness to build mindfulness.
{%tl-F5E5CC, 000000, 7%}
“You’ve got to be ready for it,” he said. “I think if I had gone two years ago, I would still be looking for a solution to my problem.”
A friend bought him a gym membership and More started walking on a treadmill, relearning how to walk in a way that keeps his pain at bay. He starts each morning soaking in a hot tub, which allows him to then transition into walking. Sometimes he still dreams of a fix, but he’s coming to grips with the reality that there may not be a solution.
“There’s no way to fix it mechanically, so my brain has to do the work and retrain my nerves to behave,” he said. “They’re sending a brain a constant signal as if there’s something wrong. It’s not accurate, it’s misfiring. So I’ve got to learn to live with it.”
For now, it’s taking small steps forward. In late March, he left town for the first time in years, visiting a friend in Portland. It’s progress, but he returned with his arm black and blue from holding the steering wheel for three hours. “I’m here because of the mountains, but it’s a constant reminder of what I can’t do,” he said. “I woke up this morning, the sun was coming up, I wanted to drive down to (Mt.) Bachelor, to at least take some pictures, but everybody would be hiking the cone, it would be depressing.”
He’s talked about moving back to New Jersey to be near his family. He worries about not contributing financially at home.
“I don’t know what the future holds, I don’t know how to make a living, I don’t know how to be happy without being physical,” he said. “I made it to the other side of opiates. I’m proud of myself for doing that.”•
Markian Hawryluk produced this special report as part of a yearlong Reporting Fellowship on Health Care Performance sponsored by the Association of Health Care Journalists and supported by The Commonwealth Fund.
“You start to think maybe it is in my head and maybe I am crazy. People start thinking you’re exaggerating everything and so you just learn to keep it to yourself.” Bill More
TAKE our survey
We’re interested in hearing about how the opioid epidemic and the public health response to it are affecting chronic pain patients and doctors, family members and addicts.
There are separate sections for patients, providers, family members and those with addictions. All responses will be held confidential and nothing will be shared without express permission.
www.bend bulletin.com/opioidsurvey
A pinkie finger test
Dr. Lorimer Moseley, a professor of clinical neurosciences at the University of South Australia, and his team, once tested the pain threshold in the pinkie fingers of professional musicians. They found that violinists and string players had much lower pain thresholds in their left pinkie fingers than in their right. But there was little difference between the two among musicians playing the piano or other instruments that require using both hands equally.
“And that’s actually not that surprising if you understand that pain is not about what’s actually happening, it’s about protection,” Moseley said. “Violinists have far more reason to protect their left hand than their right hand.”
Violinists couldn’t play very well without a little finger on their left hand, but could still hold the bow in their right without one.
“So, it would be sensible for the brain to be more protective of the left hand than it is of the right hand,” Moseley said. “Without a left little finger, you might as well change to the piccolo or something.”






